If you’ve made your initial consultation, congratulations on taking the first step! While you wait for the day of your new patient appointment, there are plenty of action items you...
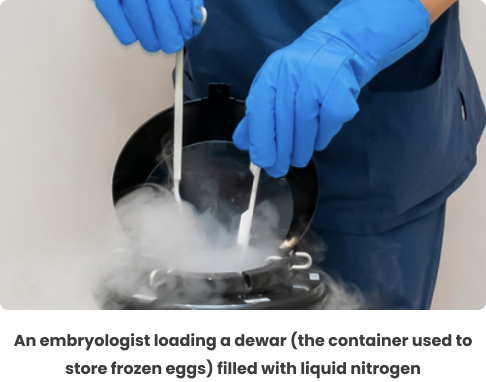
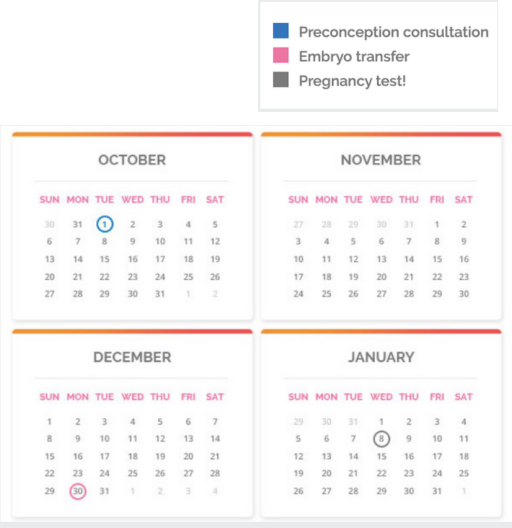
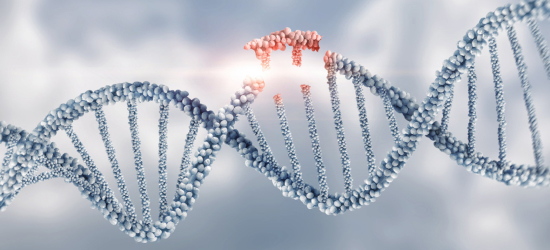
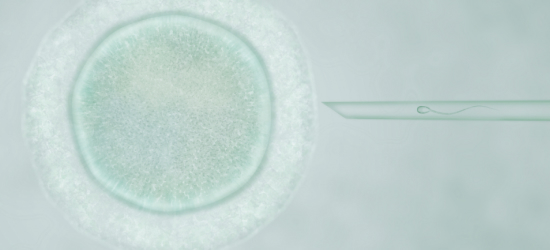
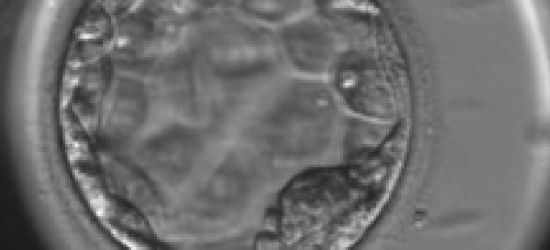
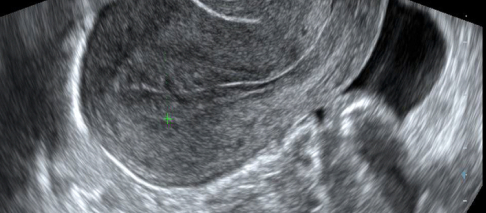
You’ve done the heavy lifting with egg retrieval and egg freezing. This page explains how to use frozen eggs – from secure storage (cryopreservation) and thawing to ICSI fertilization, blastocyst culture, optional preimplantation genetic testing, and embryo transfer-so you can plan the next steps with confidence.