Modern fertility testing at Marin Fertility Center uses best-in-class technology for a faster, gentler, and more comfortable experience. Our fertility clinic in San Francisco offers advanced diagnostic panels and modern fertility tests that minimize office visits and deliver accurate results. Discover the MFC difference and see why we are among the top Bay Area fertility clinics.
Modern Fertility Testing and Evaluation
Faster and Gentler Fertility Testing
The Importance of an Accurate Fertility Evaluation
At MFC, we emphasize the pivotal role that a precise fertility evaluation plays in shaping your entire fertility care journey. An initial, thorough diagnosis by an experienced fertility doctor is the foundation for personalized fertility solutions—including options for egg retrieval, fertility preservation, and cryopreservation of eggs and embryos. This baseline is critical for anyone considering IVF, IUI, or fertility preservation for cancer patients.
Four Key Opportunities in Modern Genetic and Fertility Testing
Genetic testing and fertility testing can be broken down into four key opportunities to maximize the chance of a healthy pregnancy. Regardless of your circumstances, every patient benefits from the first two: ovarian reserve assessment and uterine/tubal evaluation. The next two—advanced endometrial receptivity and preimplantation genetic testing—are tailored to specific reproductive needs.
Ovaries: Assessing Ovarian Reserve and Egg Supply
Old School:
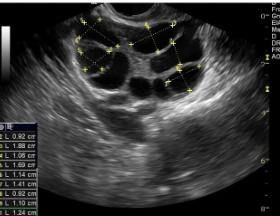
Manual follicle counts are inconsistent and prolong your exam.
MFC Approach:
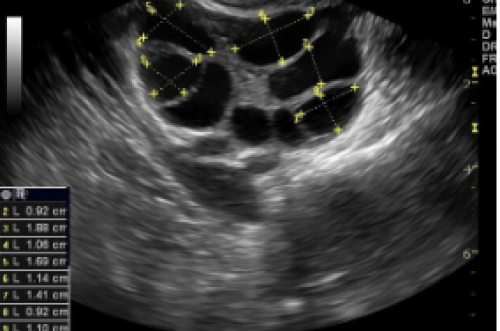
We use automated antral follicle count technology and advanced ovarian reserve testing for greater accuracy and speed. This is vital for evaluating fertility potential, especially if you’re considering egg freezing or want to know how to improve egg quality before egg retrieval.
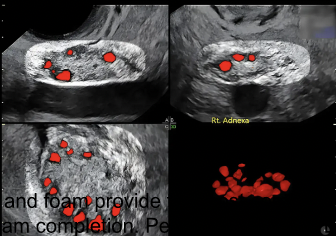
Uterus and Tubes: Modern Imaging for Fertility Testing
Old School:
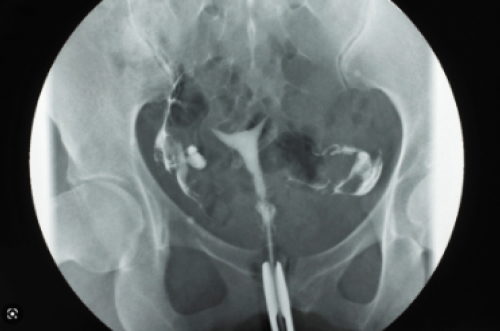
The traditional hysterosalpingogram (HSG) uses x-ray dye, which can be painful and stressful.
MFC Approach:
We offer ultrasound and FDA-approved ExEM foam, making tubal and uterine assessments safer and more comfortable. These methods support fertility preservation, identify uterine factors, and help screen for tubal blockages—essential steps in any modern fertility test or fertility evaluation.
Endometriosis and Endometrial Receptivity
Old School:

Diagnosing endometriosis required surgery.
MFC Approach:

We use non-surgical ReceptivaDx testing, completed in just minutes in-office, to assess for endometriosis and optimize endometrial receptivity. This helps guide advanced treatment options and improve IVF success rates.
Follicular Monitoring and Embryology Lab Excellence
Old School:
Manual follicle measurement could be inconsistent and time-consuming.
MFC Approach:
Computer-assisted follicle monitoring in our embryology lab offers greater consistency, supporting tailored stimulation protocols and precise timing for egg retrieval, blastocyst culture, and cryopreservation of embryos.
Male Fertility Testing and Advanced Semen Analysis
Old School:

Basic sperm counts and motility assessments miss deeper issues.
MFC Approach:
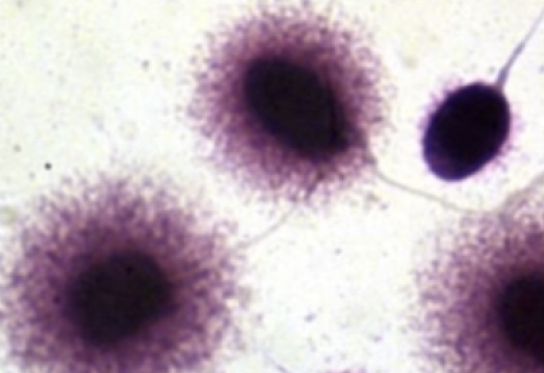
Our comprehensive male fertility evaluation includes advanced semen analysis with DNA fragmentation testing, providing essential molecular insights that conventional methods miss. This is a core part of a thorough fertility evaluation at any leading fertility clinic in San Francisco.
One-Visit Fertility Testing: The BLOOM™ Panel
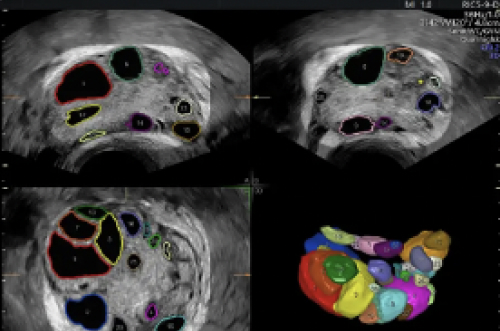
MFC’s exclusive BLOOM™ (Baseline Lining, Oviduct, Ovary, and Male testing) is a single office-visit comprehensive fertility testing panel, covering all four basic areas of reproductive endocrinology.
Over 90% of patients leave with a clear, definitive diagnosis after just one appointment—essential for planning successful fertility preservation, egg retrieval, and embryo transfer cycles.
A comprehensive fertility evaluation means that all four areas—uterine lining, oviducts (fallopian tubes), ovaries, and male factors—are tested for issues. Most patients receive a definitive diagnosis, though some may need follow-up. Fertility potential may change over time, so repeat baseline testing is sometimes recommended.
Testing the lining of the uterus includes assessing thickness, 3D structure, and endometrial receptivity—key for embryo implantation and predicting what to expect during egg retrieval or IVF.
Oviducts transport eggs, sperm, and embryos. We use the latest ultrasound-based tubal patency evaluation to ensure your fallopian tubes are open, supporting natural conception and advanced procedures like IUI and IVF.
Ovarian reserve is evaluated by ultrasound follicle count and AMH testing—crucial for assessing reproductive aging, fertility preservation, and planning any future egg retrieval.
The male fertility evaluation starts with semen analysis (volume, count, motility, morphology) and may include DNA fragmentation. Male factors are responsible for nearly 50% of infertility cases, making this step essential in all fertility testing panels.
The BLOOM™ panel includes:
- 3D pelvic ultrasound with uterine imaging and saline sonogram
- In-office tubal patency assessment
- SonoAVC antral follicle count
- Advanced semen analysis (including DNA fragmentation)
BLOOM™ is performed on cycle days 6–10 for women with regular cycles.
Digging Deeper: Immunology, Blastocyst Culture, and Advanced Fertility Testing
If standard fertility testing doesn’t reveal the answer—especially with recurrent implantation failure or pregnancy loss—we turn to immunology. Our partnership with Pregume allows us to investigate HLA mismatches, natural killer cell activity, systemic inflammation, thrombophilia, and autoimmunity.
Our embryology lab also offers advanced blastocyst culture, preimplantation genetic testing, and support for fertility preservation for cancer patients, ensuring every angle is covered.
When to See a Fertility Specialist & What to Expect During Egg Retrieval
If you’ve been trying to conceive for 12 months (6 months if over 35), or have known reproductive health concerns, schedule a fertility evaluation. Your MFC team will explain what to expect during egg retrieval, discuss options like cryopreservation of eggs and embryos, and answer any questions about fertility testing or how to improve egg quality.