Although an average ejaculate contains more than 250 million sperm, most are lost during their journey inside the female reproductive tract. When sperm reach their destination it is estimated that...
Donor Sperm
who it may be for
- Single women
- Women with female partners
- Women with a male partner who has no sperm or an unpredictable amount of sperm.
how it can be used
definitions
Anonymous sperm donor
An anonymous sperm donor refers to an individual who donates sperm to a fertility clinic or sperm bank with the intention of helping others achieve pregnancy. Typically, recipients receive information about the donor’s physical characteristics, medical history, education, and sometimes personal interests, but specific details that could reveal the donor’s identity are intentionally withheld. The anonymity aspect is designed to protect the privacy of both the donor and the recipients, providing a degree of separation in the donor-conception process.
Genetic carrier screening status
Expanded carrier screening (ECS) refers to the assessment of a donor’s genes for autosomal recessive mutations that, if shared by the sperm recipient, may lead to a disease in any offspring. ECS allows intended parents to make informed decisions, minimizing the risk of inherited conditions and promoting the health of any future offspring conceived using the donor sperm.
Known sperm donor
A known sperm donor is an individual who willingly provides sperm to assist others in achieving pregnancy, and unlike an anonymous donor, their identity is disclosed to the intended parents. This type of donor can be a friend or someone the recipients personally know. The transparency in a known sperm donation arrangement allows for a more direct connection between the donor and the intended parents, fostering open communication.
Blood type
Considering blood type in the context of donor sperm involves awareness of the donor’s blood type and the potential for Rh incompatibility between the donor and the intended parent. Rh incompatibility can lead to complications in pregnancy, so understanding both the donor’s and the recipient’s Rh status is crucial. This information allows for informed choices in selecting donor sperm to minimize the risk of Rh-related issues during the pregnancy and ensure a healthier reproductive process.
An accredited cryobank
An accredited cryobank has undergone a rigorous process to obtain accreditation, ensuring it meets industry standards and ethical guidelines for sperm donation and storage. This credentialing process involves thorough assessments of the facility’s practices, adherence to quality control measures, and compliance with legal and regulatory requirements. Choosing a credentialed cryobank provides assurance to prospective parents regarding the quality, safety, and reliability of the donor sperm, as well as the overall integrity of the reproductive services offered by the institution.
Cryostorage
Cryostorage refers to the freezing and long-term storage of sperm samples in a controlled environment, typically within a cryobank or fertility clinic. Sperm is stored in ultra-low temperatures of liquid nitrogen (-196 degrees Celsius or -321 degrees Fahrenheit) effectively halting the biological processes, maintaining the viability of the sperm cells over an extended period. In the context of donor sperm, cryostorage allows for the preservation of sperm from donors for an extended period and ensures flexibility in when it is used.
Cytomegalovirus (CMV)
Cytomegalovirus (CMV) is a common virus that is screened for in sperm donors. While CMV itself doesn’t usually cause significant issues in healthy adults, it can pose significant risks if acquired during pregnancy, potentially severely affecting the developing fetus. Donor sperm banks screen for CMV to minimize the risk of transmission and help ensure the safety of the assisted reproductive process. It is the policy of MFC to only use CMV negative sperm if the recipient is positive to past CMV infection.
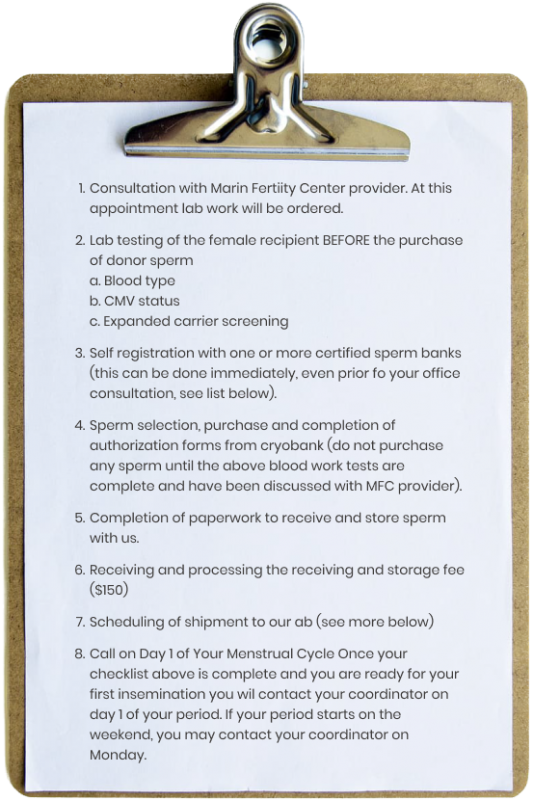
steps to complete before purchasing anonymous donor sperm
Matching
Prior to purchasing sperm, in order to match you medically, you need to know your status for 3 tests. These can be ordered by your MFC provider.
1) Your blood type
2) Your CMV status
3) Your genetic carrier status
Anonymous donor sperm pre-purchase checklist
To help organize your preparation we have put together the following checklist which can be printed or saved from here
selection of anonymous donor sperm
Patients can select sperm from a wide range of certified sperm banks. They are responsible for choosing a donor and directly paying the sperm bank for the sperm and associated shipping costs. Patients may need to review donor lists from multiple banks before finding the ideal match. It is important to note that we do not provide guidance on the selection of a specific donor, as it is a personal decision.
In cases where a patient intends to utilize donor sperm due to the intended father’s lack of viable sperm and wishes to keep this information undisclosed to the future child, the blood type of the donor becomes relevant. In such situations, it is advisable to choose a donor whose blood type matches that of the intended father.
Preparations
When choosing a donor, we advise patients to take into account the assured sperm quality offered by the bank. The quantity of actively swimming sperm provided by different banks can differ significantly. Therefore, we recommend that our patients collaborate with banks that provide a guarantee of at least 15 million motile sperm per vial following the thawing process.
There are 3 ways that sperm banks prepare their sperm
-
IUI sperm, or sperm for intrauterine insemination
In this process, the sperm bank handles the sample by eliminating seminal fluid and nonviable sperm before freezing. Once thawed, the sample retains motile sperm, suitable for direct injection into the uterus. Due to the additional processing involved, IUI sperm is sometimes pricier compared to ICI sperm. For inseminations conducted at our clinic, MFC recommends acquiring IUI-prepared sperm samples ensuring a minimum of 15 million live sperm per vial upon thawing.
-
ICI sperm, or sperm for intra-cervical insemination
The frozen sperm sample has not undergone any processing or preparation. Similar to fresh ejaculated semen, this sperm can be deposited near the cervix and naturally swims into the uterus and fallopian tubes. Patients who choose to do a home insemination frequently acquire sperm samples prepared in this way; however this preparation is not preferred for office based insemination procedures due to the presence of seminal fluid, which can trigger uterine contractions.
If a patient mistakenly purchases ICI sperm but requires an IUI or IVF procedure, our clinic can prepare the sperm for this purpose. However, this process may incur additional costs and result in some loss of sperm during preparation. -
A.R.T. sperm (“IVF Prepared”)
There are also A.R.T. sperm (“IVF Prepared”) samples available at select sperm banks for patients undergoing in vitro fertilization (IVF). As fewer sperm are required for use in assisted reproductive technology compared to IUI and ICI, these samples contain significantly fewer sperm and are consequently less expensive than insemination vials.
However we do not recommend the purchase of A.R.T. vials, regardless of the treatment. These vials contain a lower quantity of sperm than other types of samples, increasing the likelihood of insufficient sperm for our needs. If ART vials are the only ones available, consideration should be made to purchasing multiple vials.
receiving and storing frozen donor sperm in our lab
In coordination with your cryobank, our team will assist patients in the process of sending sperm and scheduling the delivery to our laboratory. Sperm is sent in a container known as a dry shipper (chilled to freezing temperatures without shipping actual liquid nitrogen). A dry shipper allows the sperm to remain safely frozen for a period of days to sometimes weeks as the shipment takes place. Shipments or drop-off deliveries are only accepted at pre-scheduled times from Monday to Friday, between 9 am to 2 pm, excluding weekends and holidays
When frozen donor sperm is received by our lab, it is placed into long term storage tanks. For individuals using the sperm in the near future, we offer a complimentary 2 week period of storage. After this 2 week window, frozen sperm is stored with us for $0.00 per month.
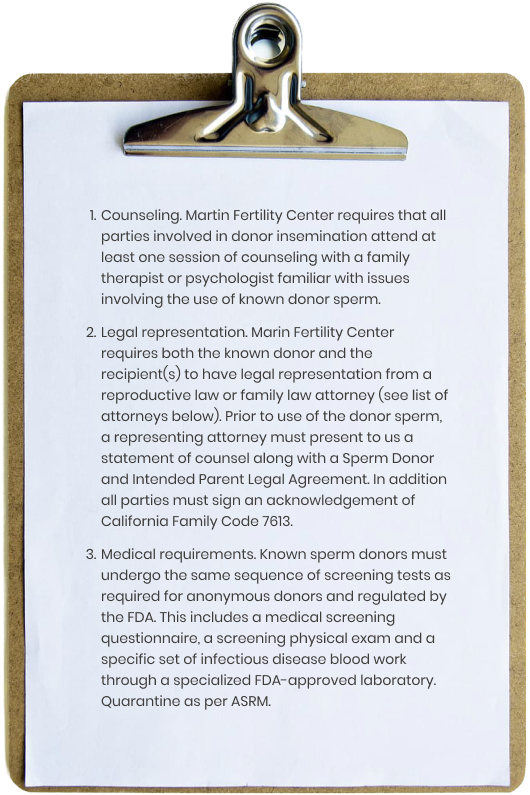
known donor sperm
Some women may consider the use of known donor sperm however this pathway does require a significant amount of extra steps, costs and time. While sperm purchased through a cryobank has been pre-screened and ready for use, known sperm donors have to undergo that process prospectively. This screening includes counseling, legal representation and a FDA-regulated screening process. Marin Fertility Center adheres to professional guidelines established by the ASRM including quarantine recommendations.
Known donor sperm checklist
FAQ
What kind of sperm prep do I need?
The type of sperm preparation needed depends on the treatment chosen (IUI or IVF). IVF is less restrictive (as less sperm is needed) and essentially any prep will work. For IUI it is important to distinguish between washed and unwashed semen (aka ICI). Washed refers to the process of isolating high-quality motile sperm away from seminal fluid, non-moving sperm and other debris. For IUI we advise targeting 10 million post wash motile sperm which means the target pre-wash amount is 20 million (roughly 50% are lost in the wash). We advise paying attention to how much volume is in a purchased vial as the volume affects the amount. (1 ml vs ½ ml vial)The specific sperm preparation method should be discussed with your providers.
What medical information should I consider?
When considering donor sperm, it’s crucial to review comprehensive medical information provided by the sperm bank. This information should include the donor’s genetic screening results, family medical history, and any relevant personal health details. Evaluating this medical information helps prospective parents make informed decisions, ensuring compatibility and minimizing the risk of hereditary conditions in the assisted reproductive process. In depth genetic counseling is available through our local Amy Vance at (415) 819-9402.
How many vials should I purchase?
The number of vials to purchase depends on various factors, including the desired number of children, the chosen method of assisted reproduction, and potential future family planning. It is generally recommended to consider purchasing an adequate supply, considering the success rates of the chosen pr
ocedure and the potential need for additional attempts. Also limited future inventory can be an issue especially if hoping for a donor-matched future sibling.
How are anonymous donors screened?
Anonymous sperm donors undergo thorough screening processes to ensure the quality and safety of donated sperm. The screening typically includes comprehensive medical examinations, genetic testing, and assessments of the donor’s reproductive health. Additionally, donors provide detailed personal information, enabling fertility clinics or sperm banks to offer recipients insights into the donor’s physical characteristics, education, and interests while maintaining the donor’s anonymity.
What should I look out for medically in the donor selection process?
In the donor selection process, it’s essential to prioritize key medical factors. Look for comprehensive genetic screening results to assess the risk of hereditary conditions, review the donor’s family medical history for any significant health trends, and consider the donor’s overall reproductive health. Additionally, pay attention to any disclosed personal health information to make an informed decision that aligns with your reproductive goals and minimizes potential health risks in the donor selection process.
Certified sperm banks
California Cryobank: www.cryobank.com
Seattle Sperm Bank: www.seattlespermbank.com
Fairfax Sperm Bank: www.fairfaxcryobank.com
Xytex: www.xytex.com
Cryos: www.cryosinternational.com
Reproductive attorneys
Shelley Tarnoff (http://tarnofflaw.com/)
159 St. James Dr.
Piedmont, CA 94611
T 510 482 2226
F 510 482 2239
Mary E Cedarblade
PO Box 477
Fairfax, CA 94978
T 415 459 8994
California AAAA Fellow Attorneys
( https://adoptionart.org/adoption-attorney-california/#!directory/xcl=1 )
Family therapists
Nancy Boughey: www.nancyboughey.com
Madeleine Katz, PsyD: www.drmadeleinekatz.com
learn more
The gold standard for success. The idea behind IVF is that, by removing several of the variables encountered during the initial steps of reproduction, the overall chance of pregnancy is...
If you’re currently trying to conceive or simply planning to become pregnant in the future, information about genetic testing options is a must. The technology behind genetic testing continues to...